RESUMEN
La polineuropatia desmielinizante aguda (AIDP) es un desorden inmune que afecta el nervio periférico produciendo
lesión axonal o mielínica. las infecciones respiratorias altas, gastrointestinales o los cuadros febriles inespecíficos
usualmente preceden este caudro clínico caracterizado por debilidad progresiva y disminución de reflejos miotendinosos. En el paciente con infección VIH la AIDP usulamnete aparece en el periodo de seroconversión cuando
el conteo de CD4 es mayor a 500 células/uL. Se presume origen infecciosos a pesar de no existir un anticuerpo
específico. reportamos dos casos de paciente con VIH y ADPI con resentación atípica. El primero con un conteo
de CD4 menos a 100 células/uL, el segundo en el contexto de síndrome de reconstitución inmunológica (IRIS).
Ambos pacientes tuvieron recuperación satisfactoria luego de tratamiento con inmunoglobulina intravenosa y
suspensión temporal del tratamiento antiretroviral respectivamente.
PALABRAS CLAVES. Síndrome de inmunodeficiencia adquirida, Polineuropatias.
Case reports
Patient 1
A 37 year old male diagnosed with human immunodeficiency virus (HIV) infection in september
2008 whose initial T lymphocyte CD4 count was 20
cells/µl on antiretroviral therapy with zidovudine,
lamivudine and nevirapine started on mid october,
presented in early february 2009 with a one week
history of rapid progressive strength and sensory
loss on lower extremities with further involvement
of both hands. On admission to the hospital the neurological examination disclosed proximal and distal
reduced strength which Medical Research Council
(MRC) score was 3/5. In addition, tendinous reflexes
were absent and severe sensory loss for all modalities
was noted on stocking distribution. By this time his
T lymphocyte CD4 count was 46 cells per micro
liter and HIV viral load was lower than 40 copies/
ml. Other serum test included complete blood count
(CBC), liver enzymes, renal and thyroid profile,
vitamin B12, folic acid, lactate and creatin kinase
(CK) determinations which results were reported as
normal. Cerebrospinal fluid (CSF) analysis showed
0 cells, protein 231 mg/dl and glucose 66mg/dl.
Cultures for bacteria, fungus and deoxyribonucleic
acid (DNA) polymerase chain reaction (PCR) for
cytomegalovirus (CMV) varicella zoster virus (VZV)
and tuberculosis were negative. Additionally CSF
venereal disease research laboratory (VDRL) was
non reactive and CSF HIV viral load was lower
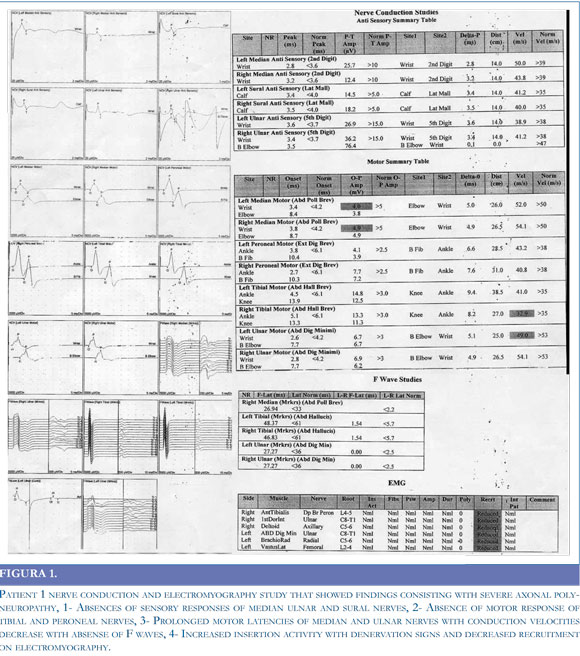
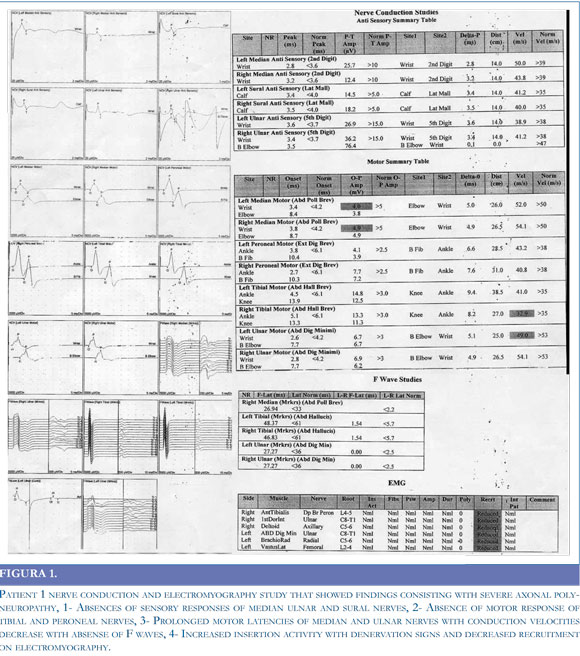
than 200 copies/ml. A diagnosis of Guillain Barre
syndrome was made further supported by nerve
conduction study and electromyography of four
limbs that demonstrated demyelination with reduced
motor conduction velocities and prolonged distal
motor latencies. Furthermore F wave responses were
markedly reduced and EMG showed reduction in
motor unit recruitment. (Figure 1) The patient was
commenced on a five-day course of intravenous
immunoglobulin (IVIG) in a dose of 0.4 g/kg
body weight a day with no side effects. The patient
started improving his neurological condition shortly
after completion of IVIG administration, reaching
complete recovery following two months. During
all this time the patient continued his antiretroviral
regimen with no changes.
Patient 2
A 46 year old male with HIV infection diagnosed
in February 25, 2008 in the setting of P. Jirovecci
pneumonia, T lymphocyte CD4 count of 49 cells/µl and HIV viral load higher than 1000000 copies
/ml, started antiretroviral therapy with zidovudine,
lamivudine and efavirenz in the third week of March
08. He noted one month later a six days history of
difficulty to walk due to loss of strength on both
lower extremities with no sensory involvement.
Other medications included trimethoprim sulfamethoxasole and fluconazol. On admission to the
hospital his physical examination only showed mild
quadriparesis with absent achillean and patellar
reflexes. Workup laboratories included CBC, electrolytes, liver enzymes, renal function, thyroid profile,
vitamin B12, folic acid, and lactate, all reported as
normal. In addition his most recent T lymphocyte
CD4 count was 221 cells/µl and the HIV viral load
was lower than 50 copies /ml. CSF analysis showed
1 cell, protein 157 mg/dl and glucose 54 mg/dl,
cultures were negative; VDRL non reactive and
CMV/VZV DNA detection by PCR was negative.
CSF HIV viral load was lower than 200 copies per
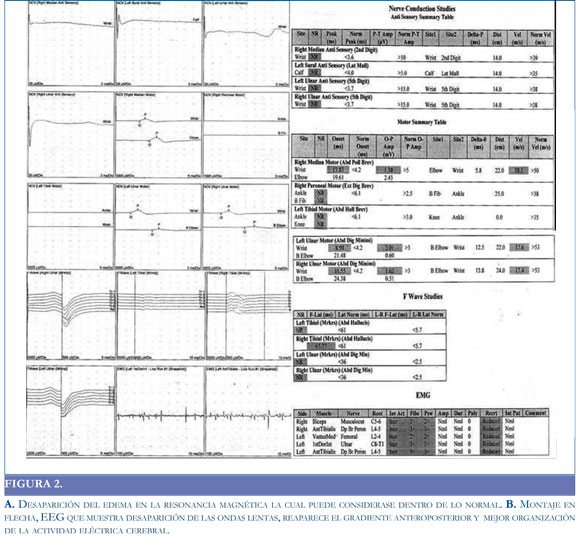
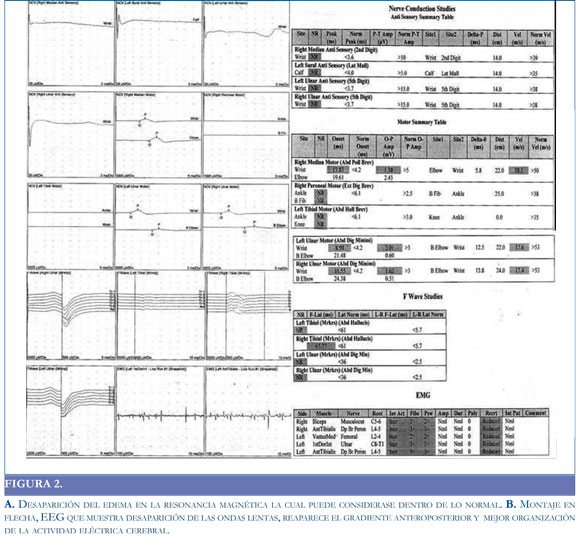
ml. One week later nerve conduction studies plus
EMG of lower extremities were done showing
reduced F waves responses and motor conduction
velocities. EMG showed only mild reduction in
motor unit recruitment (Figure 2). A diagnosis of
acute inflammatory demyelinating polyneuropathy
(AIDP) in the setting of an immune reconstitution
syndrome was made. Because the symptoms were
not disabling the patient severely at all, it was decided
to continue with his antiretroviral regimen without
modification. No further worsening of symptoms
was noted by the patient and his neurological examination showed a rapid improvement of the strength
one month after starting an intensive program of
physical therapy. Currently -June 2009- he has no
neurological symptoms.
DISCUSSION
Cell-mediated immunity is known to play an
important role in the pathogenesis of GBS. The cha-
racteristic initial stage of this entity is associated with demyelinization related to the action of macrophages, with multifocal distribution in the nerves. The
main action of T cells appears to be the impairment
of the integrity of the blood-nerve barrier by the
action of metalloproteinases, in addition to influence
the recruitment of other immune cells o such as
macrophages, Schwann cells and fibroblasts (1).
Acute AIDP is an uncommon disorder in the setting of HIV infection that usually has been seen shortly
after seroconversion when the T lymphocyte CD4
count is higher than 500 cells/µl (2), this disorder
seems to be immune mediated depending on a
possible over activity of T and B lymphocyte cell
population. Biopsy and autopsy findings have been
contradictory regarding the presence or absence of
perivascular lymphocyte infiltration in GBS. The fact that no lymphocytes are detected in nerves
suggests that the changes mediated by antibodies
are important, in agreement with the pathogenetic
mechanism proposed for the onset of GBS, which
occurs after infections, as is the case or Campylobacter jejuni which is associated with antibodies to
GM1 and GQ1b gangliosides. These gangliosides
share epitopes with the lipopolysaccharide coat of
some strains of this bacterium (3).
There are few HIV/AIDP cases published in the
literature whose CD4 count is lower than 50 cells
and co infection especially by cytomegalovirus has
been ruled out either by CSF DNA detection by PCR
or clinical course.2, 4 The exact mechanism of thiphenomenon is unknown since it could be assumed
that patients with not enough T lymphocyte CD4
count are unable to mount a competent immune
response. However it is hypothesized that alteration
of T cell homeostasis induced lymphopenia could
be permissive for the disruption of self tolerance
and autoimmune disease may occur in lymphopenic
patients (4).
The first case is an example of this scenario
which clinical outcome behaved similar to Guillain
Barre syndrome in HIV seronegative patients that
usually respond to IVIG or lasmapheresis (5).
Some authors promote performing plasmapheresis followed by IVIG in the setting of HIV infection
but cases where the CD4 count is lower than 100
cells /µl administration of gancyclovir or foscarnet
should be considered until CMV polyradiculopathy
is excluded (6).
The second case displays an immune reconstitution syndrome (7) that elicited AIDP in context of
recent onset of antiretroviral therapy with a CD4
count lower than 100 cells/µl. In this situation an
autoimmune disorder can promotes damage of
peripheral nerves explained by the role of T cells
contributing to the selection of natural self-reactive
antibody repertories whose expression of immuoglobulin M (IgM) and immunoglobulin G (IgG)
toward some self-antigens depends on the number
of T CD4 lymphocytes (8).
The course of HIV is characterised by a decreasing CD4 count and a rising viral load. There is loss
of lymphocytes to a level where secondary immune
responses are lost to both primary and recall
antigens.9 On commencement of HAART viral
suppression is sufficient to allow regeneration, by
clonal expansion of the remaining clones, of these
immune responses.10 This has resulted in an immunological response to self or pathogen, where there
was previously anergy, the aptly named immune
reconstitution syndrome.11,12. To our knowledge
there are no more than 10 case reports published
of AIDP associated to immunologic reconstitution
inflammatory syndrome (IRIS) in the setting of HIV
infection (9-12). Therapeutic approaches include conservative measures, steroids plasmapheresis or
temporary suspension of antiretroviral therapy (12).
Acknowledgments
Special thanks are given to to Pontificia Universidad Javeriana school of Medicine, Dr Joe Fernando Muñoz for his clinical work and editorial assistance
and Dr Julio Cesar Castellanos, for supporting
Infectious Diseases Unit at Hospital Universitario
de San Ignacio in Bogota Colombia South America.
REFERENCES:
1. PITHADIA AB, KAKADIA N. Guillain-Barré
syndrome (GBS). Pharmacol Rep. 2010; 62: 220-32.
2. BRANNAGAN TH 3RD, ZHOU Y. HIV-associated Guillain-Barre syndrome. J Neurol Sci. 2003: 15; 208: 39-42.
3. QURESHI AI, COOK AA, MISHU H, KREN
DEL DA. Guillain- Barre´ syndrome in immunocompromised patients: a report of three patients
and review of the literature. Muscle Nerve. 1997; 20:
1002-1007.
4. MISHRA BB, SOMMERS W, KOSKI CL,
GREENSTEIN JI. Acute inflammatory demyelinating polyneuropathy in the acquired immune deficiency syndrome. Ann Neurol. 1985; 18: 131-132.
5. KRUPICA JR T, FRY TJ, MACKALL CL. Autoimmunity during lymphopenia: a two-hit model. Clin
Immunol. 2006; 2: 121-128.
6. BURNS TM. Guillain-Barre syndrome. Semin
Neurol. 2008; 28: 152-67.
7. MARKARIAN Y, WULFF EA, SIMPSON DM. Peripheral neuropathy in HIV disease. AIDS Clin
Care. 1998;10:89-91, 93, 98.
8. SHELBURNE SA 3RD, HAMILL RJ. The
immune reconstitution inflammatory syndrome.
AIDS Rev. 2003; 5: 67-79.
9. STAHL D, LACROIX-DESMAZES S, MISRA N,
KARMOCHKINE M, KAVERI SV, COSTAGLIOLA
D, ET AL. Alterations of self-reactive antibody
repertoires in HIV disease: an insight into the role
of T cells in the selection of autoreactive B cells.
Immunol Lett. 2005; 99: 198-208.
10. TEO EC, AZWRA A, JONES RL, GAZZARD
BG, NELSON M. Guillain--Barre syndrome following immune reconstitution after antiretroviral
therapy for primary HIV infection. J HIV Ther.
2007; 12: 62-63.
11. FUJISAKI G, KAMI M, MURASHIGE N, KISHI
Y, HORI A, CHIZUKA A. Guillain-Barre syndrome associated with rapid immune reconstitution following allogeneic hematopoietic stem cell
transplantation. Bone Marrow Transplant. 2006; 37:
617-619.
12. PILIERO PJ, FISH DG, PRESTON S, CUNNINGHAM D, KINCHELOW T, SALGO M, ET
AL. Guillain-Barré syndrome associated with
immune reconstitution. Clin Infect Dis. 2003; 36:
e1111-114.